Central Line Care
A Central Venous Catheter (CVC) provides venous access for patients requiring short/long term therapies. To many patients the catheter is an important lifeline, therefore it is imperative that the catheter is handled and maintained correctly. The use of central venous access devices is a well-established practice in both primary and secondary care; ensures appropriate venous access for patients requiring many different forms of treatments including chemotherapy, parenteral nutrition, IV antibiotic therapy, IV fluid replacement, blood product transfusion, venous blood sampling and measurement of central venous pressure. They can also be used for renal dialysis and bone marrow transplantation, as well as for patients with poor venous access.
The term Central Venous Catheter (CVC) refers to an intravenous catheter whose internal tip lies in a large central vein, access is usually via the superior or inferior vena cava.
There are various types of CVC but common to all is the concept that the tip of the catheter floats freely within the bloodstream in a large vein parallel to the vein wall, so that blood flow is maximised, and physical and chemical damage to the internal walls of the vein are minimised.
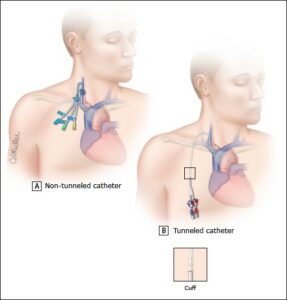
They can be classified as Non-Tunnelled, Tunnelled, peripherally inserted and totally implantable, depending on how the catheter is inserted.
Types of CVC:
- Non-tunnelled (also known as Percutaneous and Non-Cuffed CVC): the catheter is inserted by puncturing directly into the skin and vein without tunnelling the subcutaneous tissue.
- Duration: short term but can be used long term.
- Indications:Difficult intravenous access; infusion of irritant drugs, vasopressors, and inotropes; short term total parenteral nutrition.
- Examples: Multi-lumen short-term CVC; Percutaneous introducer; Temporary haemodialysis catheter (Vascath®)
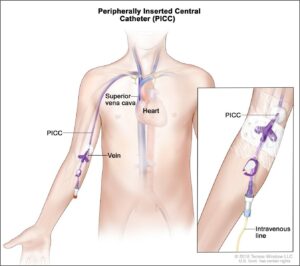
- Peripherally inserted (known as PICC line – Peripherally Inserted Central Catheter): the catheter is inserted into a vein of the upper arm.
- Duration: Medium term
- Indications:Difficult intravenous access; blood sampling; medium term drug administration (e.g., antibiotics); administration of irritant drugs (such as chemotherapy); total parenteral nutrition
- Note: requires adequate peripheral venous access; the tip of the PICC line rests in the superior vena cava at the junction of the right atrium.
- All patients should have clear documentation of the external length of the catheter visible outside the body at time of placement in their medical notes and a record of this measurement should be written in a standard letter for the Community Nurse. This will enable any practitioner caring for the PICC to determine if the catheter has moved since the insertion.
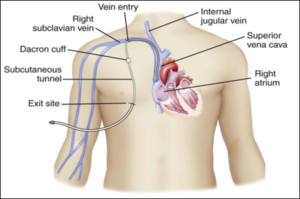
- Tunnelled: line in which the proximal end of the catheter is tunnelled subcutaneously from the insertion site and brought out through the skin at an exit site.
- Duration: long term (months to years, for intermittent or continuous access)
- Indications:Long term administration of irritant drugs (such as chemotherapy); long term IV medication.
- Examples: Hickman®, Broviac® and permanent haemodialysis catheters (e.g. Perm-Cath®, Hemosplit®, or Equistream®).
- Note: the catheter has a cuff to reduce line colonisation along tract; the catheter tip is placed at the junction of the superior vena cava and the right atrium.
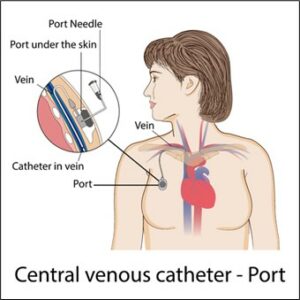
- Totally implantable: (also known as Implanted Venous Access Device (IVAD), or “Port”): line that is surgically placed into a vessel, body cavity, or organ and is attached to a reservoir or “port” located under the skin.
- Duration:long term (months to years, for intermittent or continuous access)
- Indications:Long term intermittent access (e.g. patients with regular hospital admissions with poor intravenous access); administration of irritant drugs (such as chemotherapy)
- Examples: Portacath®
- Note: a Non-coring needle (Huber needle) is needed to access the device; the catheter tip is placed at the junction of the superior vena cava and the right atrium.
Assessment
Prior to any catheter care, it is important to observe the catheter and the surrounding area for any signs of complications and to complete a short assessment: Observe for:
- Pain – arm, shoulder neck or chest
- Redness
- Swelling, engorged veins in the arm, neck, or chest.
- Exudate, redness, pain at exit site Pyrexia or a history of rigors post flushing.
- Any history of rigors or feeling unwell post flushing
- Dressing allergy – redness, blistering, itching, pain under the dressing.
- Migration (PICC line)
- Leaking of fluid beneath the dressing.
- Cuff exposure (CVC)
Any signs or symptoms of complications should be reported to the referring hospital without delay.
Diagrams
Revised: January 2025
Version: 2 (Review)
Source: Expert Care Manager
 Back
Back